Nosokinetics
Problems in the light: look in the dark
A queueing network model with blocking:
analysis of congested patients flows in mental health systems.

Naoru Koizumi
Assistant Professor, School of Public Policy,George Mason University, Arlington, Virginia, USA.
The current trend toward downsizing and closing of state mental health institutions has led to an over-utilization of many local mental health facilities. This problem has often been exacerbated by a shortage of long-stay psychiatric hospitals and community-type accommodations. Many patients are spending extra days in unnecessarily intensive facilities, leading to congestion of these facilities. In the present study, an open queueing network model with blocking is applied to analyze such congestion processes (Figure 1). Here “blocking” denotes situations where patients are turned away from accommodations to which they are referred, and are thus forced to remain in their present facilities until space becomes available.
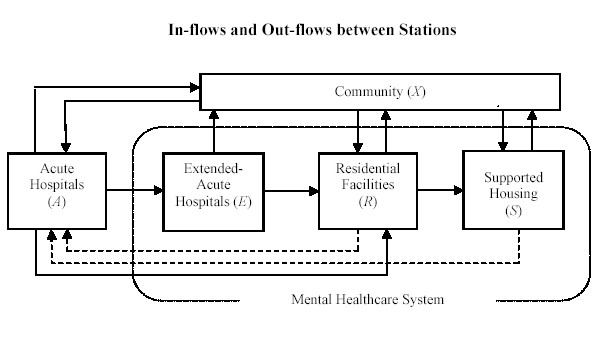
Figure 1 Model of the in-flows and out-flows in the mental healthcare systerm.
Although traditional queueing models have been used in numerous healthcare studies, the inclusion of blocking is rarely found. This study specifically examines blocking in interrelated mental health facilities, including (a) acute hospitals (where patients wait to enter extended acute hospitals), (b) extended acute hospitals (where patients wait to enter residential facilities), and (c) residential facilities (where patients wait to enter supported housing). The Philadelphia mental health system is used as a case study. This system has experienced severe congestion problems since 1992.
In the theoretical portion of this study, a queueing network model of the Philadelphia system is constructed and analyzed both in terms of steady-states behavior and transient behavior via numerical simulations. These theoretical results are then compared with the observed congestion levels in Philadelphia. The single most important finding is that, in contrast to popular perception, system congestion is not always a simple cumulative effect of shortages across all facility types.(Figure 2)
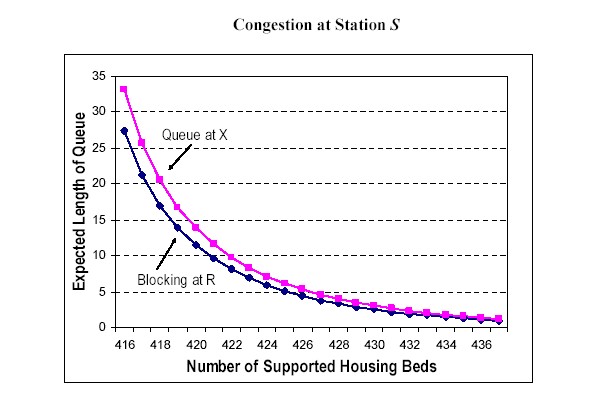
Figure 2 Impact of small changes in the number of supporting housing beds on queue length in the community (X) and “blocking“ in residential care.
In the Philadelphia case, it is shown that system-wide congestion is due primarily to shortages in one specific facility type, namely, supported housing. Here the shortage of supported housing in Philadelphia has created “upstream blocking” of patients at both extended acute hospitals and residential facilities. Perhaps the most important policy implication of this analysis is that removal of such facility-specific bottlenecks may often be the most cost-efficient way to reduce congestion in the system as a whole.
Reference:
The PhD Thesis is available on-line; see also the paper Koizumi, N., E. Kuno, et al. (2005). "Modeling Patient Flows Using a Queuing Network with Blocking." Health Care Management Science 8(1): 49-60.
Some navigational notes:
A highlighted number may bring up a footnote or a reference. A highlighted word hotlinks to another document (chapter, appendix, table of contents, whatever). In general, if you click on the 'Back' button it will bring to to the point of departure in the document from which you came.Copyright (c)Roy Johnston, Peter Millard, 2005, for e-version; content is author's copyright,