Nosokinetics
Outpatient Models for a Diagnosis and Treatment Centre
John Bowers and Gillian Mould, University of Stirling
(comments to e-mail addresses?)
Introduction
Staff from the University of Stirling have been working with Hospital Trusts to produce tools to support the modernisation of health services. Past studies have explored day surgery and inpatient care. A recent project has focussed on outpatients, developing models to assist in the design of a Diagnosis and Treatment Centre (DTC).A planning tool has been constructed which allows managers to select the specialties for inclusion in the DTC and explore the consequences. The model produces estimates of resource usage for outpatient treatment: within the DTC; remaining in the acute hospital and within the community. The model combines forecasts of activity demand in a range of scenarios with changes in care pathways to estimate the requirements for radiology, pathology, therapies, endoscopies, ambulances, clinic space and staffing.
Assimilating data from different sources
Data were obtained from a variety of sources: centralised IT systems, local systems, special manual data collection exercises, observation and interview. Data were analysed to determine the relationship between specialties and the various services in order to appreciate the impact of possible transfers to the DTC from the existing hospital. Considerable effort was dedicated to validating the data and comparing them to staff’s personal experiences; this provided an essential check and also helped establish confidence in the basis of the analysis.
New pathways and their implications for the DTC
Four representative specialties were examined in detail: cardiology; colorectal, elective orthopaedics and respiratory medicine. Discussions were held with staff: consultants, nurses, physiotherapists, other clinical staff and PCT managers to establish the current pattern of treatment for a number of common conditions. Treatment pathways were produced for these.A range of possible future modifications to the treatment regime was identified by examining practice in other hospitals: the Department of Health Action-on sites highlighted a number of new methods of organisation and clinical practice which will improve services for patients. The possible alternative treatment pathways were discussed with staff, from the Acute hospital and Primary Care, to establish their feasibility and the implications for the design of the DTC.
The layout and the resource requirements of the DTC should be specified to facilitate the effective implementation of new pathways. Some new pathways may require additional resources to ensure that services are available to meet the patients’ needs but other pathway revisions can reduce the resource requirement. There were numerous revisions to the hip and knee pathway. Figure 1 shows the pathway before revisions and Figure 2 shows the revised pathway for use in the DTC.
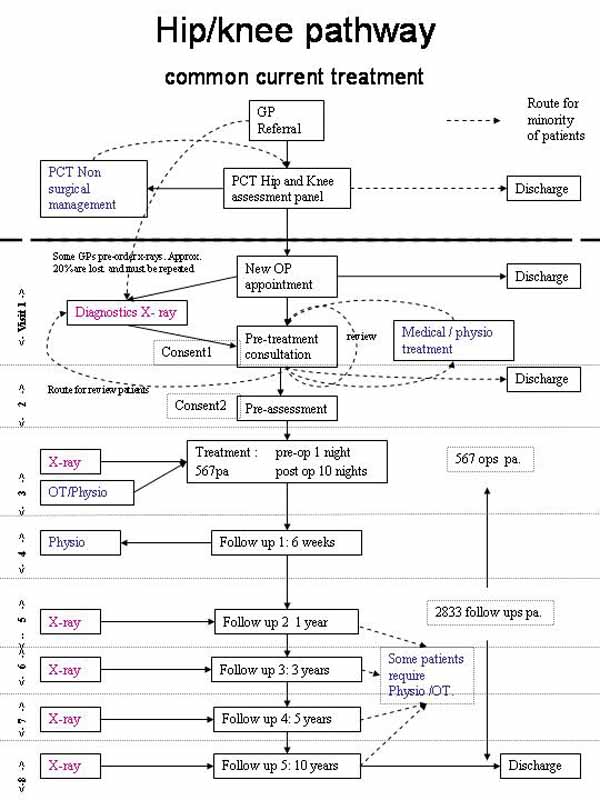
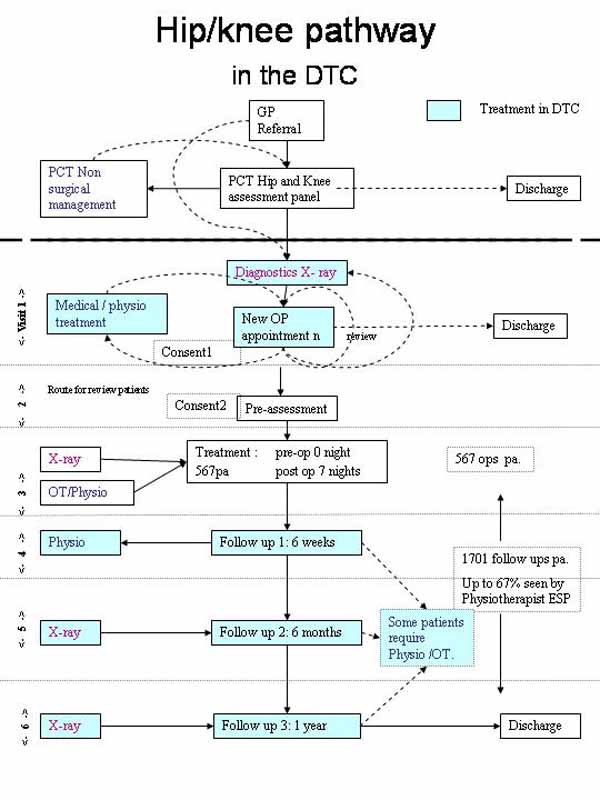
In Primary Care, a recent initiative of triaging referrals and offering non-surgical management to less urgent cases has delivered a high conversion to surgery rate (63%) for new outpatient appointments. In time, this should reduce the number of inappropriate referrals. Actions have been taken to reduce the number of follow up patients seen by consultants. A three-appointment one-year follow up plan was suggested, as recommended by the British Orthopaedic Association,. Consultants are keen to follow up patients over a 10 year time period to gain feedback on the long term results of their treatment, however this feedback can still be obtained by following up just a sample of patients over 10 years. A physiotherapist ESP is also undertaking routine follow-ups. The implications of these changes on resource use are shown in Table 1:
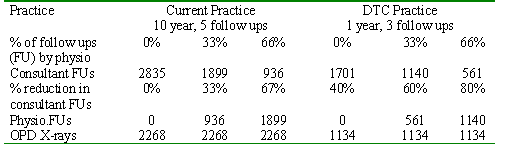
Table 1: Implications of changes in the hip and knee pathway (567 procedures p.a.)
Other developments in pathways do not reduce the number of stages of treatment, but allow diagnostics and consultations to take place in the same visit, increasing the convenience for the patient and also reducing the administration overhead in the clinic. The experiences in these examinations of new pathways were used in conjunction with benchmarking analyses to determine key parameters, such as the follow-up rates, for input into the capacity planning exercise. Further studies explored changes in ‘did not attend’ DNA rates and the organisation of clinics and the consequences for the DTC.
Forecasts of future demand
The possible future demand was estimated using the trends in referrals in each directorate, A number of different forecasts were considered, including an assumption of the demand remaining at the current level and another assuming national trends, as noted in Table 2. Additional scenarios were explored with varying assumptions about the impact of changing practice on follow-up, DNA rate and the potential for transfer of activity into primary care.
Table 2 A selection of scenarios
Exploring the impact on services
The model was used to produce detailed predictions of resource requirements for each scenario. An example is shown in Table 3, this shows the resource requirements for different types of radiology, therapy and pathology by the DTC, outpatients in the existing hospital, primary care Accident and Emergency and inpatient services. The overall implications for outpatient attendances, clinics and services from different scenarios are compared in Table 4.
Table 3 Estimates of services assuming 2007/8 demand (scenario 4)
Table 4 Selected scenarios & estimates of outpatient attendances for 2007/8
scenario 1 = current demand
scenario 4 = directorate trends + reductions in follow-up & dna rates
scenario 7 = national trends + reductions in follow-up & dna rates
NB. All figures used in this document are illustrative rather than actual predictions of demand.
A complete picture
The study combined a diverse range of data into a set of models which aimed to provide a more complete picture of the present and possible future organisation of outpatient care. The study was more than a cold, quantitative capacity planning analysis: it incorporated visions of future patterns of care and involved a range of staff from both the acute hospital and primary care, helping to establish a better basis for designing the DTC.
References:
(Refs to come)
Some navigational notes:
A highlighted number may bring up a footnote or a reference. A highlighted word hotlinks to another document (chapter, appendix, table of contents, whatever). In general, if you click on the 'Back' button it will bring to to the point of departure in the document from which you came.Copyright (c)Roy Johnston, Ray Millard, 2005, for e-version; content is author's copyright,